“Five people die with sepsis every hour in the UK, 25, 000 hospital admissions for sepsis are related to children and 40% of people with sepsis never fully recover Sepsis (UK Sepsis Trust).”
What is Sepsis?
Sepsis can be hard to spot especially in people with communication problems, dementia, learning disabilities and the young and elderly. Its symptoms can be vague and similar to other conditions such as the flu (NHS UK). Patients more at risk of developing sepsis are the young and elderly along with people with chronic conditions, but everyone is at risk.
Early recognition of sepsis has been associated with a better outcome as sepsis is aggressive, quick and can engulf the body. Sepsis can become a life-threatening condition. It is caused by the body’s response to an infection. The body normally releases chemicals into the bloodstream to fight an infection. In Sepsis this chemical release can become out of balance, taking over the body, triggering changes that can damage multiple organ systems. Sepsis can progress into septic shock resulting in multiple organ failure and death. (MayoClinic, 2018).
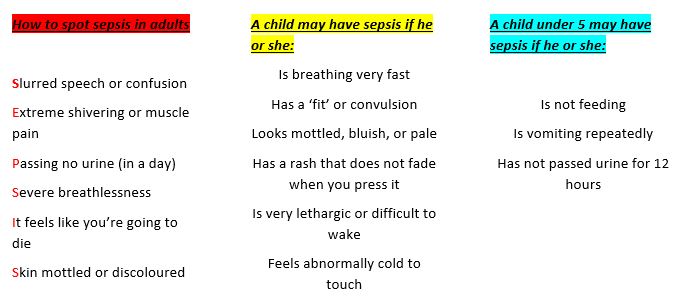
How can we spot it? (As per UK Sepsis Trust)
The National Institute for Health and Clinical Excellence have developed a sepsis risk stratification tool and guideline which will be of benefit for all clinical practitioners to follow as a guide for diagnosis / support for adults and children. To see more, click here
By diagnosing sepsis early, the sepsis 6 can be implement within a hospital setting more quickly. It has been shown that early implementation of the sepsis 6 can reduce mortality. The sepsis 6 is a medical bundle compiling of blood cultures, full blood count and lactate, IV fluid challenge, IV antibiotics, oxygen and urine output monitoring (UK Sepsis Trust). Lets save lives and improve outcome by identifying sepsis early.
References:
- MayoClinic (2018), Sepsis, https://www.mayoclinic.org/diseases-conditions/sepsis/diagnosis-treatment/drc-20351219
- NHS UK (2019), Sepsis https://www.nhs.uk/conditions/sepsis/
- UK Sepsis Trust, https://sepsistrust.org/about/about-sepsis/
Written by Jen Clayton (ECG, Freelance trainer), Wednesday 26th February 2020